Prevalence of neurological disorders in French bulldog: a retrospective study of 343 cases (2002–2016)
Background
The French Bulldog (FB) is a canine breed originating from France. The numbers of FBs have markedly increased in recent decades. In Europe, FB has significantly gained in popularity over the last few years. For example, annual registrations of FBs have quadrupled over the past 15 years in France [1], and in the United Kingdom, 14,607 new registrations to the Kennel Club were recorded in 2015 versus 526 in 2006 [2]. In North America, FB was the 6th most popular breed in the United States in 2014 [3], and the 9th most popular breed in Canada in 2015 [4]. Due to the brachycephalic and chondrodystrophic body conformation resulting from selective inbreeding, a high prevalence of various diseases has been described in this breed, including several neurological conditions [5]. These include not only myelopathies such as compressive vertebral malformations [6], spinal arachnoid diverticula [7] and intervertebral disc disease [8], but also encephalopathies such as brain tumours [9] or non-infectious encephalitides [10]. To the authors’ knowledge, no study has yet reported the prevalences and distributions of different neurological disorders in FB or has described a specific neurological condition in this emerging breed. The primary objective of this epidemiological study was therefore to report the prevalences of different neurological conditions in a large population of FBs presented for neurological signs at a major referral centre. A secondary objective was to identify epidemiological characteristics regarding specific diseases in this singular breed.
Methods
Case selection
Case records of all French bulldogs presented for neurological signs (including spinal pain) at our institution between January 1st, 2002 and January 1st, 2016 were retrospectively reviewed. Dogs were included if they met all the following inclusion criteria: (I) neurological clinical signs, including isolated spinal pain, (II) complete available records and (III) a definitive etiological diagnosis. The only exception was the inclusion of young dogs presented for an auditory function screening, as several animals were asymptomatic. Dogs that did not present actual neurological clinical signs or signs mimicking a neurological condition but related to another cause (e.g. orthopaedic or ophthalmic conditions) were otherwise excluded. Similarly, animals with only a neuroanatomical diagnosis (e.g. “T2-L2 myelopathy”, or “cauda equina syndrome”) were not included in the study.
Neurological diseases classification
When a dog was presented at our institution two times or more for neurological conditions, only the first one for which the dog was presented was taken into account. Similarly, when two concomitant neurological diseases were diagnosed at the same time on the same dog (i.e. with one being an incidental finding), only the one responsible for the clinical signs was retained. To facilitate data processing, each case was assigned to one of the following neuroanatomical categories, according to the definitive diagnosis: encephalopathy, myelopathy, peripheral nervous system (PNS) & muscles disorder, and unclassified neurological condition. Diseases unrelated to one of the above-listed categories, such as paroxysmal dyskinesia, tremors syndromes and congenital deafness were grouped together under “unclassified neurological conditions”.
Criteria used for the diagnosis of specific diseases
Definitive diagnoses for each patient were then established by a board-certified neurologist based on patient’s signalment and history, clinical findings and appropriate ancillary tests, according to the current knowledge for each condition. Ancillary tests comprised miscellaneous blood testing (including biochemical analyses, serum bile acids measurement, complete blood count, electrolytes, hormonal testing, serology), cerebrospinal fluid (CSF) analysis, PCR screening for various endemic infectious agents of the nervous system, cytology and histology of various tissues, otoscopy, bacterial culture on various materials, muscles and nerves biopsies, myelography, cross-sectional imaging (Computed tomography [CT] and magnetic resonance imaging [MRI] scans), and electrodiagnostics (electromyography, nerve conduction studies and brainstem auditory evoked response [BAER]). Two MRI devices were used during the study period: a low-field (0.2 T) device prior to 2013, and a high-field device (1.5 T) after 2013. Criteria allowing diagnoses of diseases the most frequently expected are listed in the following sections.
Brain diseases
When available, brain tumours were diagnosed based on histological examination. In cases where a histological examination was not performed, MRI criteria were used. An intracranial glioma was defined as an intra-axial solitary lesion, more or less enhancing after paramagnetic intravenous contrast media administration, accompanied or not by surrounding oedema and/or mass effect [11]. Similarly, pituitary neoplasia diagnosis was based upon histological analysis and/or CT or MRI imaging features (masses well-delineated in the pituitary area, more or less invading the surrounding parenchyma with contrast enhancement), along with consistent biochemical or ultrasonographic abnormalities (hypercortisolism, bilateral adrenal enlargement etc. [12]). When the diagnosis was achieved through imaging criteria, the term “suspected neoplasia” was therefore used to refer to these diseases.
In cases of absent histopathological diagnosis, meningoencephalitis of unknown (MUO) origin was diagnosed based on the following previously described criteria: Focal or multifocal clinical signs of brain disease, T2-weighted multifocal intra-axial hyperintense lesions with variable T1-weighted contrast enhancement on MRI, mononucleated pleocytosis on CSF analysis, and exclusion of endemic infectious diseases [13]. Idiopathic epilepsy diagnosis was based upon the International Veterinary Epilepsy Task Force consensus, and included normal inter-ictal examination, normal brain MRI and CSF analysis, as well as a normal comprehensive biochemistry profile investigating metabolic causes of seizures, including serum bile acid and electrolytes [14]. Criteria allowing diagnosis of otogenic bacterial encephalitis included consistent central nervous system (CNS) clinical sings, middle/inner ear MRI and/or CT abnormalities, T1- weighted meningeal and/or brain parenchyma enhancement on MRI, inflammatory CSF (with or without bacterial culture), and a positive response to antibiotic treatment. The diagnosis of metabolic encephalopathies was based on clinical signs suggestive of brain disease, consistent MRI findings and an identified metabolic origin on blood analysis (e.g. hepatic or renal failure) [15].
Myelopathies
Intervertebral disk herniation was diagnosed either by CT, MRI or myelography associated with consistent clinical signs and onset. The distinction between Hansen type I and type II IVDH was based upon a combination of clinical and imaging criteria and the perioperative appearance of herniated material in dogs that underwent surgical treatment, as described in previous studies. Hansen type I IVDH was suspected on CT if hyperdense presumed disk material was observed in the intervertebral space and/or within the vertebral canal, along with subsequent spinal cord compression on transverse planes and/or epidural fat displacement [16]. It was suspected on MRI if the disk had extruded through the annulus fibrosus, and appeared as a compressive extradural hypointense (either in T2 or T1-weighted) single lesion, mostly lateralized and dispersed from either side of the intervertebral space [17]. Hansen type I was suspected during surgery if calcified/mineralized nucleus pulposus was extruded in the vertebral canal and/or under the dorsal longitudinal ligament [18].
Spinal arachnoid diverticulum (SAD) was defined on myelography or CT-myelography as contrast-filled, teardrop shaped expansion of the subarachnoid space, with a possible abrupt interruption of the contrast column immediately after the lesion. On MRI, it was defined as a T2-weighted hyperintense, T1-weighted and/or FLAIR hypointense lesion of the subarachnoid space [19].
When histological examination was not performed, usual previously described imaging criteria were used to diagnose spinal tumours, especially regarding the relationship between the lesion and the subarachnoid space [20].
PNS & muscle disorders
Otitis interna was defined as the combination of clinical signs suggestive of a peripheral vestibular syndrome, evocative imaging findings either with CT (fluid-filled tympanic bulla) or MRI (fluid-filled tympanic bulla and loss of the normal T2-weighted hypersignal of the inner ear), and evidence of inflammation/infection on bulla cytology. Congenital deafness was defined as hearing loss or deficits since birth, confirmed by a consistent BAER study [21].
Data acquisition and statistical analysis
The clinical database of the institution was searched using the clinical software (CLOVIS, 4Dv13) and appropriate keywords. When information was missing from numerical records, the paper files were retrieved if available. For each case fulfilling the inclusion criteria, data were recorded using a form created with EpiData v3.1 Software (Lauritsen J.M., Bruus M. & Myatt M., UK/ Denmark). Information regarding file number, age, sex, body weight, duration of clinical signs, and definitive diagnosis were collected. Complete data were then exported into an Excel 2010 spreadsheet (Microsoft Office 2010, Excel 2010) for further statistical evaluation. Percentages for each subpopulation were calculated with a 95% confidence interval, using the asymptotic/Wald method (for groups in which n x p > 5, where n is the number of individuals in the concerned subpopulation, and p the estimate prevalence rate), or the exact binomial/Clopper-Pearson method (for groups in which n x p < 5, EpiTools, AusVet Animal Health Services). The χ2 statistical test (or Fisher’s exact test when appropriate) was used to assess the statistical association between age (taken as a binary variable with appropriate cut-off) or sex, and the occurrence of IVDH or meningoencephalitis of unknown origin. Odds Ratio (OR) were calculated to quantify the association between sex and occurrence of MUO, age and occurrence of IVDH, and were provided with their 95% confidence interval (CI). A P-value < 0.05 was considered significant. Statistical tests were performed using a website dedicated to statistical analysis (BiostaTGV, http://marne.u707.jussieu.fr/biostatgv/). A receiver operating characteristic (ROC) curve analysis was performed to determine a cut-off value for the age that best discriminated the presence (versus absence) of meningoencephalitis of unknown origin. The optimum cut-off value was determined with Youden’s index criteria. An appropriate statistical software was used for the ROC analysis (SAS Software, version 9.3).
Results
Study population
Between 2002 and 2016, 2846 FBs were presented at our institution (representing 3.1% of all dog breeds), all chief complaints and all departments combined. Over this period of time, FB was the sixth most popular breed after standard poodle (4.1% of all dogs breeds), German shepherd (4.2%), Labrador retriever (6.2%), Yorkshire terrier (6.8%) and mixed-breed dogs (10.1%). A total of 533 FBs (18.7% of the 2846 FBs) were presented for suspected neurological signs. During the same period, a total of 88,863 dogs (FB excluded) were presented at our institution, of which 10,150 (11.4%) were admitted for neurological clinical signs.
Among the 533 FBs presented for neurological clinical signs, 25 were excluded because the clinical examination failed to identify a neurological disorder. A further 165 animals were excluded because of incomplete files and/or absence of definitive diagnosis. In the end, 343 FBs with a confirmed neurological disease and a precise diagnosis were included in the statistical analysis, representing 12% of all FBs presented to the institution during the study period. The whole case selection procedure is detailed in Fig. 1. Two concomitant neurological conditions were diagnosed in only 9 dogs at the time of presentation.
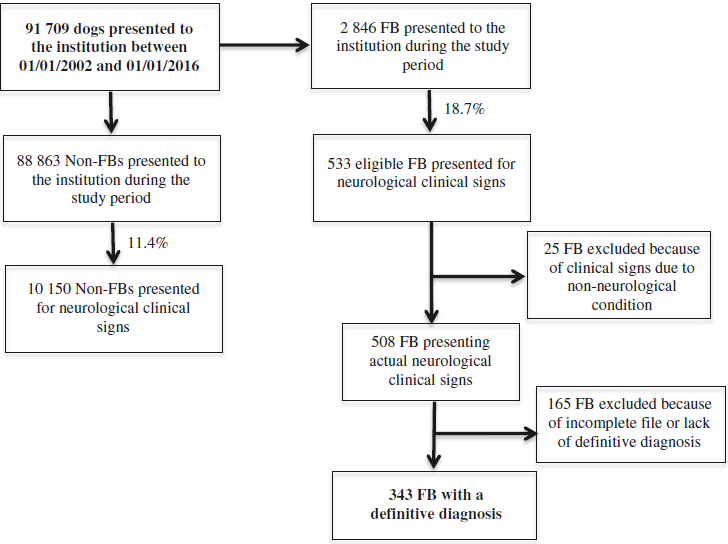
Fig. 1 Data flow diagram illustrating the case selection procedure of the 343 French bulldogs (FB) selected from the general hospital population between 2002 and 2016, and presenting neurological clinical signs and a definitive diagnosis
 Overall distribution of neurological diseases
Overall distribution of neurological diseases
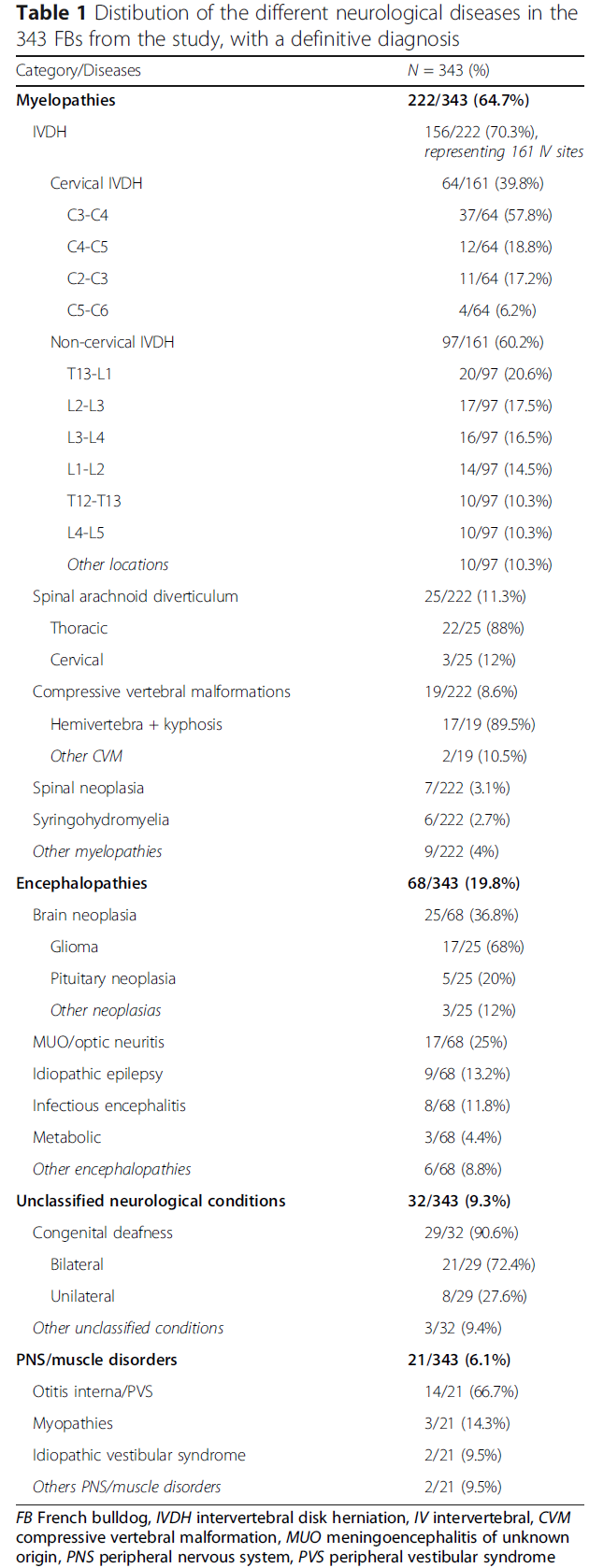
In total, 64.7% of the 343 dogs presented a myelopathy (n = 222 dogs, 95% CI 59.7–69.8%), 19.8% presented an encephalopathy (n = 68, 95% CI 15.6–24.0%), 9.3% presented an unclassified condition (n = 32, 95% CI 6.5– 12.9%) and 6.1% presented a PNS/muscle disorder (n = 21, 95% CI 3.8–9.2%). The median age of the FBs in this study was 4.0 years (range from 0.2 to 14.5 years). There were 188 males (including 19 castrated dogs) and 155 females (including 64 spayed females). All the results are detailed in Table 1.
Myelopathies distribution
Hansen type I intervertebral disk herniation was the most common myelopathy, with 70.3% documented cases (n = 156 dogs, 95% CI 64.3–76.3%). IVDH accounted for 45.5% (95% CI 40.2–50.8%) of all the neurological conditions, and for 5.5% of all FBs presented to our institution during the study period (95% CI 4.6–6.3%). Five dogs presented two IVDH at the time of presentation, representing a total of 161 sites of disk herniation. Cervical IVDH accounted for 39.8% of all IVDH (n = 64, 95% CI 32.2–47.3%), whereas thoracolumbar and lumbar locations represented 60.2% of IVDH (n = 97, 95% CI 52.7–67.8%). There was no significant association between sex and IVDH (p = 0.95). When cervical and thoracic/lumbar IVDH were taken together, most dogs (80.8%, 95% CI 74.6–87.0%) were more than 3 years old. Age was significantly associated with IVDH, since 81% of FBs affected by IVDH were 3 years old or 533 eligible FB presented for neurological clinical signs 508 FB presenting actual neurological clinical signs 343 FB with a definitive diagnosis 165 FB excluded because of incomplete file or lack of definitive diagnosis 91 709 dogs presented to the institution between 01/01/2002 and 01/01/2016 88 863 Non-FBs presented to the institution during the study period 10 150 Non-FBs presented for neurological clinical signs 11.4% 18.7% 2 846 FB presented to the institution during the study period 25 FB excluded because of clinical signs due to non-neurological condition Fig. 1 Data flow diagram illustrating the case selection procedure of the 343 French bulldogs (FB) selected from the general hospital population between 2002 and 2016, and presenting neurological clinical signs and a definitive diagnosis more, compared to 64% of dogs affected by another myelopathy (OR = 2.4, 95% CI 1.2–4.5, p < 0.01).
Spinal arachnoid diverticulum was the second most common myelopathy, with 11.3% of dogs affected by this condition (n = 25, 95% CI 7.4–16.2%). SAD represented 7.3% of all diseases of the study (95% CI 4.5–10.0%). Compressive vertebral malformation was diagnosed in 8.6% of dogs with myelopathy (n = 19, 95% CI 5.2–13.0%), followed by a neoplastic condition (either spinal or vertebral neoplasia) in 3.2% of dogs (n = 7, 95% CI 1.3–6.4%), syringomyelia in 2.7% of dogs (n = 6, 95% CI 1.0–5.8%), and ischemic myelopathy in 1.8% of dogs (n = 4, 95% CI 0.05–4.5%). The remaining disorders of the spinal cord were acute non-compressive nucleus pulposus extrusion (n = 3), immune-mediated myelitis (n = 1), and lumbosacral spinal cord dermoid sinus (n = 1).
Cervical intervertebral disk herniation
The median age of dogs affected by cervical IVDH was 4.2 years (range from 1.5 to 10 years), and the median weight was 12.4 kg (range from 8 to 19 kg). Cervical hyperesthesia, often pronounced, was observed in 82.8% of dogs presenting cervical IVDH (n = 53, 95% CI 73.5–92.0%). The most commonly affected site in the cervical region was C3-C4 (57.8% of cervical IVDH, n = 37, 95% CI 45.7–69.9%) followed by C4-C5 (18.8%, n = 12, 95% CI 10.1–30.5%) and C2-C3 (17.2%, n = 11, 95% CI 8.9–28.7%). An epidural hematoma/haemorrhage was observed in 3 cases that underwent cervical ventral slot surgery.
Thoracolumbar intervertebral disk herniation
Among these non-cervical IVDH (n = 97), 68 were located in the thoracolumbar (T3-L3) region and 29 were located in the lumbosacral (L4-S) region. The median age of FBs affected by thoracic and lumbar IVDH was 4 years (range from 1.7 to 13 years). The median weight was 12.4 (range from 4.5 to 18 kg). The most commonly affected intervertebral spaces in this group of dog were T13-L1 (20.6%, n = 20 95% CI 12.6–28.7%), followed by L2-L3 (17.5%, n = 17, 95% CI 10.0–25.1%), L3-L4 (16.5%, n = 16, 95% CI 9.1–23.9%) and L1-L2 (14.5%, n = 14, 95% CI 7.4–21.4%). Finally, T12-T13, L4-L5 and other intervertebral locations regrouped 10 dogs each (representing 10.3% of thoracolumbar IVDH each, 95% CI 4.3–16.4%). An extradural haemorrhage and/or hematoma was observed during cross-sectional imaging and/or surgery in 27.8% (n = 27, 95% CI 18.9–36.8%) of all cases diagnosed with thoracic or lumbar IVDH, regardless of the affected disk location.
Spinal arachnoid diverticulum
Concerning SAD, 88.0% (n = 22, 95% CI 75.3–100%) were located in the thoracolumbar (T3-L3) region. More than three quarters of the thoracolumbar SAD cases were located between T9 and T12 (77.3%, n = 17, 95% CI 59.8–94.8%). In the remaining 12.0% (n = 3, 95% CI 0.0–24.7%) of animals affected by this condition, a cervical (C1-C5) location of the SAD was observed. No SAD was found in the caudal cervical (C6-T2) or lumbosacral (L4-S) segments. In addition, a vertebral malformation (n = 12) or a mild IVDH (n = 4), at the level or distant from maximum 2 to 3 vertebral bodies to the SAD, was identified in 64.0% (n = 16, 95% CI 45.2– 82.8%) of all cases. The median age of FBs affected by SAD was 4.5 years (range from 1 to 10.7 years).
Compressive vertebral malformations
Concerning the 19 dogs clinically affected by congenital vertebral malformations, 17 presented with hemivertebrae (89.5%, 95% CI 75.7–100%) associated with a major kyphosis responsible for a compression of the spinal cord. The most commonly affected vertebrae were T6, T7, T8, and T10 (with 3 abnormal vertebrae for each). Five FB presented with two or more malformations. One dog presented with a wedge-shaped vertebrae and one dog presented with L6-L7 spina bifida.
Encephalopathies distribution
Brain neoplasia
A suspected brain neoplasia was observed in 36.8% of FBs affected by an encephalopathy (n = 25, 95% CI 28.6–53.3%), with a glioma, either suspected or confirmed, being the most common (n = 17, 68% of all neoplasias 95% CI 49.7–86.3%). Five FBs presented a pituitary macroadenoma (n = 5, 20.0% of neoplasias 95% CI 6.8–40.7%). The three remaining animals were affected by intracranial lymphoma, malignant intracranial peripheral nerve sheath tumour of cranial nerve III, or suspected osteosarcoma of the calvarium. Three gliomas and 2 pituitary macroadenomas were confirmed histologically (either with biopsies or post mortem examinations). The median age of FBs with brain neoplasia was 9.0 years old (range from 5 to 14.5 years).
Meningoencephalitis of unknown origin
Meningoencephalitis of unknown origin represented 25.0% of the encephalopathies (n = 17, 95% CI 15.3– 37.0%). The median age of FBs affected by MUO was 2.25 years (range from 0.8 to 6.5 years). Among the 68 (19.8%) FBs that presented an encephalopathy, MUO was more frequently observed in females than in males (OR = 7.1, 95% CI 2.0–25.2, p < 0.01). ROC curve analysis enabled us to determine that the cut-off age that best discriminated the presence versus the absence of MUO was 5.5 years, with a sensitivity of 60.7% and a specificity of 94.1% (Area under the curve = 0.76). Therefore, by using this cut-off, 94.1% of FBs less than 5.5 years old presented with clinical signs related to an encephalopathy were affected by MUO, whereas 60.7% of FBs of 5.5 years old or more presented with the same clinical signs were not affected by this condition.
Other encephalopathies
Regarding other conditions, idiopathic epilepsy represented 13.2% of encephalopathies (n = 9, 95% CI 6.2– 23.6%), and bacterial encephalitis associated with otitis media/interna 11.8% (n = 8, 95% CI 5.2–21.9%). The remaining encephalopathies were metabolic encephalopathies (n = 3, two hepatic encephalopathies, and one uraemic encephalopathy), congenital hydrocephalus (n = 2), cannabinoid intoxications (n = 2), ischemic stroke and degenerative encephalopathy (n = 1 for each condition).
Other neurological conditions distribution
Among the unclassified neurological disorders (n = 32), 90.6% of FBs presented congenital deafness (n = 29, 95% CI 80.5–100.0%). Bilateral deafness was detected in 72.4% (n = 21, 95% CI 56.1–88.7%) of animals presenting congenital deafness, versus 27.6% for the unilateral form of the condition. Among all FBs presented with congenital deafness, 79.3% were white or had white in their coat (n = 23, 95% CI 64.6–94.1%). Idiopathic head tremors were observed in 2 animals, and narcolepsy/cataplexy in a single case.
Among PNS/muscles disorders (n = 21), 66.7% of animals presented an otitis interna with neurological signs (see below, n = 14, 95% CI 46.5–86.8%), 14.3% presented a myopathy (n = 3, 95% CI 3.0–36.3%), with one case of each the following conditions: immune-mediated polymyositis, ischaemic neuromyopathy and corticosteroids-induced myopathy. Two animals presented an idiopathic acute vestibular syndrome, one case presented a chronic steroidresponsive polyneuropathy, and one case presented a malignant peripheral nerve sheath tumour. Among the FBs affected by otitis media/interna, all animals were presented with a peripheral vestibular syndrome, eight cases had concurrent ipsilateral facial paralysis, and four cases had a concurrent Horner syndrome.