Interstitial idiopathic pulmonary fibrosisand Sick-Sinus-Syndrome in a West Highland white terrier dog
An eleven-year-old West Highland white terrier treated for a Sick-Sinus-Syndrome since 2 years with a VVIR pacemaker was presented for exercise intolerance and panting due to interstitial idiopathic pulmonary fibrosis. Diagnosis was made before death by radiography, echocardiography and histology of lung biopsies. The follow-up was done before the dog died, 95 days after diagnosis. Necropsy was performed on heart and histology on sinus node also.© 2016 AFVAC. Published by Elsevier Masson SAS. All rights reserved.
Fibrose pulmonaire interstitielle idiopathique et Sick-Sinus-Syndrome chez un chien West Highland white terrier
Un chien West Highland white terrier mâle de 11 ans, traité auparavant pour un Sick-Sinus-Syndrome avec un pacemaker de type VVIR, est présenté pour une intolérance à l’effort et un essoufflement. Une fibrose interstitielle pulmonaire idiopathique du Westy est diagnostiquée du vivant de l’animal à l’aide de radiographies, d’une échographie cardiaque et d’un examen histologique sur des prélèvements biopsiques pulmonaires. Le suivi est effectué jusqu’au décès du chien, 95 jours après le diagnostic. Un examen nécropsique est réalisé sur le cœur, ainsi qu’un examen histologique de la région du nœud sinusal. © 2016 AFVAC. Publié par Elsevier Masson SAS. Tous droits réservés.
Description and case history
Nash, an 11-year-old male West Highland white terrier(WHWT) dog, weighing 9.5 kg, was presented for exercise intolerance and panting when at rest. The dog had beenfollowed for 2 years (since 2011) for Sick-Sinus-Syndrome which had been diagnosed after episodic weakness associated with marked irregular bradycardia, and treated byimplanting a VVIR pacemaker (ventricular pacing, ventricular sensing, inhibition response and rate-adaptive) with aunipolar epicardial pacing wire.
Arrhythmia was confirmed and a complete pre-operative evaluation was performed at the time of diagnosis (Holter examination, echocardiography, biological examination, thoracic radiographs) before implanting the pacemaker. A control echocardiogram was obtained one year later (in 2012). The animal no longer presented any symptoms at this time (complete disappearance of syncope).
Clinical examination
The animal was alert on admission. Mucous membranes were pink, with a capillary refill time of less than 2 seconds. Respiratory auscultation revealed inspiratory crackles, most audible at end-inspiration, of great intensity, bilateral and diffuse (‘‘Velcro Crackles’’), associated with moderate polypnea (respiratory rate of 45 cycles per minute). Cardiacauscultation demonstrated a left-sided apical grade 2/6 systolic murmur and a right-sided apical grade 2/6 systolic murmur.
The cardiac rhythm was generally regular. Some occasional irregularities were noted, probably secondary torhythm changes linked to pacemaker triggering. The heart rate was between 70 and 80 beats per minute. Abdominal palpation was normal, together with the rest of the clinical examination.
Clinical history
An 11-year old male West Highland white terrier, already being followed for Sick-Sinus-Syndrome, treated by pace-maker implantation two years earlier, was presented for exercise intolerance and moderate polypnea at rest. The only anomalies detected in the clinical examination were moderate polypnea, left and right-sided apicalgrade 2/6 systolic murmurs and ‘‘Velcro’’ type pulmonary crackles.
Hypotheses
The hypotheses were as follow :
- breathlessness during effort, moderate polypnea, associated with left-sided apical systolic murmur of grade 2/6and respiratory noises most audible at the end of inspiration, of strong intensity, bilateral and diffuse, maybe secondary to a pulmonary edema (left heart failure) secondary to a degenerative mitral valve disease;
- in view of the epidemiological context (age, predisposition of terrier breed), an interstitial pulmonary fibrosis was also possible, which would explain the ‘‘Velcro Crack-les’’. The grade 2/6 right-sided apical systolic murmur could, in this case, correspond to tricuspid regurgitation, which would suggest pulmonary arterial hypertension(PAH) or a degenerative tricuspid valve disease;
- other pulmonary conditions (bacterial pneumonia, respiratory disorder, parasites, etc.) can also be responsible for respiratory symptoms. A pulmonary hemorrhage was unlikely due to the reported absence of injury or ingestion of anticoagulant substances;
- finally, endocarditis could be responsible for the heart murmurs but seemed unlikely.
Complementary examinations
Thoracic radiographs
The principal hypotheses were explored by thoracic radiography (Fig. 1). A right cardiomegaly was noted (possibly secondary to PAH). A fine, smooth, interstitial pattern of the entire lung field was demonstrated.


Figures 1A and 1B. Pulmonary radiographs.
A. Right side view. Bulging of the cranial aspect of the cardiac silhouette (arrows), increased area of contact between the heart and sternum, and moderate diffuse interstitial pulmonary opacity. VHS = 11.5; NV = 8.7—10.7.
B. Frontal view, ventrodorsal projection. Rounding of the right side of the cardiac silhouette (arrows), ‘‘inverted D’’ appearance, with displacement of the heart apex towards the left hemithorax. No left cardiomegaly or signs of pulmonary venous congestion. The pacemaker sensor, placed on the left ventricle, is visible on both images. VHS: mean vertebral heart scale from Buchanan JW, Bucheler J. Vertebral scale system to measure canine heart size in radiographs. J Am Vet Med Assoc 1995;206:194—199.
These lesions were more visible on the mid-thoracic region, causing a blurring of the vascular structures and indicative of damage to the pulmonary interstitium.
There were no signs of left congestivecardiac failure.
Echocardiographic and Doppler examination
The two murmurs and the right cardiomegaly highlighted on the thoracic radiographs were explored using ultrasonic echocardiography (Table 1).
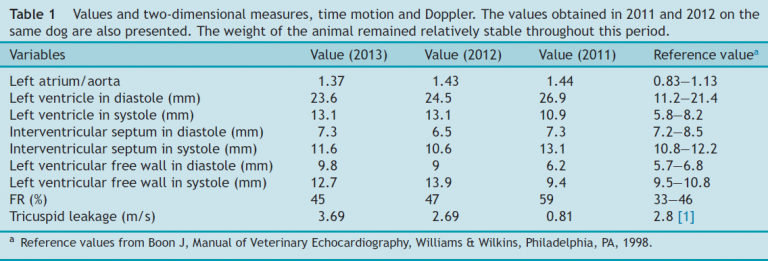
The two-dimensional echocardiographic examination showed normal valve morphology. Doppler color and continuous modes revealed very mild mitral insufficiency of weak velocity. Tricuspid regurgitation was noted. This had already been detected in the previous echocardio-grams but this time the tricuspid flowrate was significantly higher (Vmax = 3.69 m/s versus 2.69 m/s; normal values[NV] < 2.8 m/s) 1.
The pressure gradient between the right ventricle and right atrium was calculated using the modified Bernoulli equation. The result, added to the right atrial pressure value (and in the absence of pulmonary stenosis), corresponded to the systolic pulmonary arterial pressure(PAPs) (PAPs = 64.5 mmHg; NV < 30 mmHg) 1. The estimated right atrial pressure was 10 mmHg (atrial dilation only, with no right cardiac insufficiency) 1. Thus the diagnosis was moderate systolic PAH 1.
Diagnosis
The complementary examinations revealed right cardiomegaly associated with moderate systolic PAH, and diffuse interstitial pulmonary lesions. Given the observed symptoms, age of the dog and particular breed, an idiopathic pulmonary fibrosis of WHWT was strongly suspected. Pulmonary biopsies were scheduled to confirm this diagnosis at day 30 (see follow-up).
A pre-anesthetic assessment (complete blood count, biochemical analyses, and electrolyte and coagulation panel) was performed before doing the biopsies. No significant abnormalities were apparent. Apartial pulmonary lobectomy of the right caudal lobe was performed by thoracoscopic surgery. Amoxicillin—clavulanic acid (Kesium®) at 10 mg/kg twicea day (BID) PO was delivered for 5 days. Histopathological examination of the biopsies confirmed the diagnosis of idiopathic interstitial pulmonary fibrosis of WHWT (Fig. 2).



Prognosis
The prognosis for interstitial pulmonary fibrosis in the medium and long term is ‘‘reserved’’, with a median survival time of 32 months (2—51 months) 2. To date, no prognosis has been described for animals with interstitial pulmonary fibrosis and Sick-Sinus-Syndrome (even equippedwith a pacemaker).
Treatment
A calcium channel inhibitor (diltiazem, 1.5 mg/kg/day PO,Tildiem®) was prescribed to reduce the pulmonary arterialpressure (PAP).
Follow-up
Control at 30 days (date of the lung biopsies)
The owners reported a slight improvement in breathlessness since implementation of the treatment.
Thoracic radiographs revealed a definite worsening of the pulmonary lesions. The diltiazem treatment was continued.
Control at 75 days
The owners reported considerable breathlessness associated with severe bouts of coughing. The clinical examination revealed a restrictive dyspnea associated with frequent cyanosis and ‘‘Velcro Crackles’’.
This recurrence of symptoms motivated a control echocardiographic examination, which revealed accentuation of the right-sided remodeling: increased right atrialsize and observation of paradoxical motion of the septum.
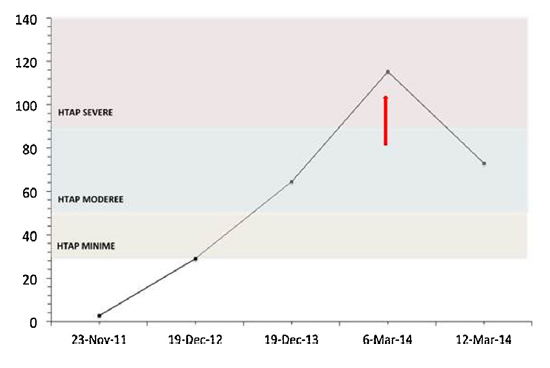
The PAPs had increased considerably (VmaxTric = 5.13 m/s;NV < 2.5 m/s, PAPs = 115.2 mmHg; NV < 30 mmHg) 1. The estimated right atrial pressure was 10 mmHg (no signs of right-sided cardiac insufficiency).
The treatment was therefore adapted.
Furosemide (2 mg/kg BID PO, Dimazon®) and benazepril (0.5 mg/kg/dayPO, Benakor®) were added to prevent possible right-sided congestion and to treat the remodeling. Pimoben-dane (0.125 mg/kg BID PO, Vetmedin®) and sidenafil(1.25 mg/kg/day PO, Viagra®), to replace the diltiazem, were also prescribed to control the PAH.
Control at 81 days
The animal was clinically stable. The control echocardiogram showed a diminition of PAPs (VmaxTric = 3.97 m/s;NV < 2.8 m/s, PAPs = 73 mmHg; NV < 30 mmHg) (Fig. 3) 1.
The same treatment was continued.
Death
The dog died 95 days after presentation following a severe worsening of dyspnea. A cardiac necropsy was performed, followed by histopathological examination of the ventricles and atria, particularly the sinus node (Fig. 4).
The results indicated considerable fatty infiltration of the sinus node region.