Introduction
Mitral endocardiosis is a chronic degenerative disease of the mitral valvular apparatus. It is characterised by myxoid degeneration with distortion of the free side of the leaflets. This distortion is responsible for deficient functioning of the valve and regurgitation. This leads to left heart insufficiency. This is the most common canine heart disease. Aged male dogs of small breeds are mainly affected [1,2]. However this disease has also been described in large breed dogs [3,4].
This clinical case describes chronic mitral valve disease in a large breed dog.
Clinical case
A 13 year old male Saluki weighing 25kg was presented for lethargy and difficulty breathing of a few days duration. Vaccinations were up to date. Mitral insufficiency had been diagnosed by another veterinarian a year earlier by echocardiography. Enalapril (0.5 mg/kg divided BID) had been given since. Rectal temperature was within normal limits. Capillary refill time was increased to 4 seconds. There was effort intolerance and symptoms were present even at rest. Respiration was dyspnoeic and the rate was increased (35 breaths per minute). The femoral pulse was thready and a pulse deficit was noted. The heart rate was high (about 180 to 190 beats per minute). Rhythm was irregular. A high intensity (4/6) holosystolic left sided apical heart murmur was heard. Respiratory sounds were increased; crackles were mostly heard during the end of inspiration.
The main differential diagnosis was congestive cardiac insufficiency with pulmonary oedema, mitral failure, and arrhythmia. Diagnostic tests were performed to evaluate all the symptoms.
Right lateral (figure 1) and dorso-ventral (figure 2) thoracic radiographs revealed bilateral cardiomegaly (Buchanan’s vertebral scale = 13 ; normal = 9.7 +/- 0.5 [5] ; the transverse diameter was more than 2/3 of the total diameter of the thorax).
 Figure 1: right lateral thoracic radiograph: left-sided cardiomegaly, venous densification, and alveolar pulmonary oedema.
Figure 1: right lateral thoracic radiograph: left-sided cardiomegaly, venous densification, and alveolar pulmonary oedema.
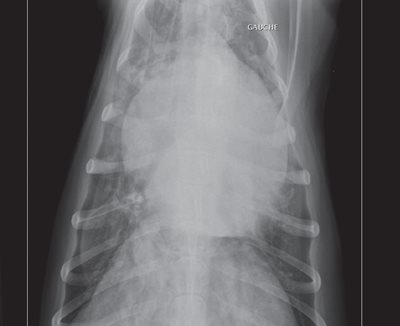 Figure 2: dorso-ventral thoracic radiograph: cardiomegaly and alveolar pulmonary oedema.
Figure 2: dorso-ventral thoracic radiograph: cardiomegaly and alveolar pulmonary oedema.
The size of the left atrium was particularly increased. The tracheo- vertebral angle was decreased. Pulmonary venous densities were present on the lateral view (figure 1). The pulmonary parenchyma showed interstitial and alveolar densities consistent with alveolar pulmonary oedema (figures 1 and 2).
These radiographs confirmed the diagnosis of congestive disease with pulmonary oedema.
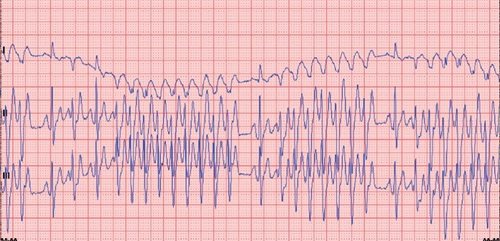 Figure 3: 6-lead electrocardiogram, 25 mm/s, 10 mm/mV: paroxysmal left ventricular extrasystoles.
Figure 3: 6-lead electrocardiogram, 25 mm/s, 10 mm/mV: paroxysmal left ventricular extrasystoles.
An electrocardiogram (6 Leads, 25 mm/s, 10 mm/mV) (figure 3) revealed an increased and highly irregular heart rate (about 250-260 beats per minute). Electrocardiographic ventricular morphologies were as follows:
- Sinus supraventricular morphology (normal complexes like complex no 3 for example);
- Paroxystic right ventricular morphology (enlarged complexes like complex no 2 example);
- Intermediate morphology (fusion complexes ie. mixed morphology between normal and enlarged complex no 4 for example).
All these changes lead to the conclusion of an intermittent left ventricular tachycardia (with series of left ventricular extrasystoles).
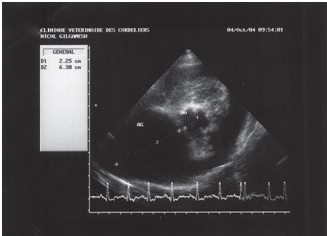
Figure 4: echocardiography (two-dimensional mode), right parasternal short axis image, transaortic view: left atrial dilatation.
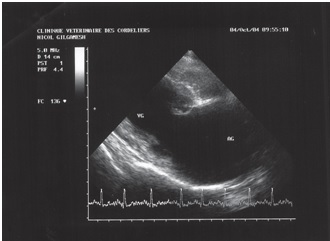 Figure 5: echocardiography (M-mode), right parasternal short axis image, transventricular view: left systolic and diastolic ventricular dilatation.
Figure 5: echocardiography (M-mode), right parasternal short axis image, transventricular view: left systolic and diastolic ventricular dilatation.
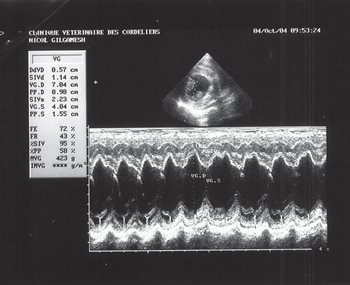 Figure 6: echocardiography (two-dimensional mode), right parasternal long axis image, four-chamber view: view of the mitral valve during diastole.
Figure 6: echocardiography (two-dimensional mode), right parasternal long axis image, four-chamber view: view of the mitral valve during diastole.
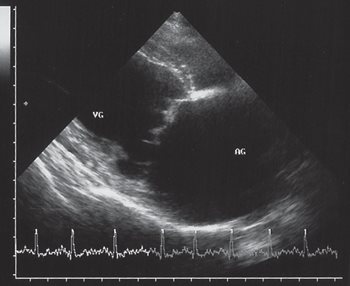 Figure 7: echocardiography (two-dimensional mode), right parasternal long axis image, four-chamber view: view of the mitral valve during systole, minor prolapse.
Figure 7: echocardiography (two-dimensional mode), right parasternal long axis image, four-chamber view: view of the mitral valve during systole, minor prolapse.
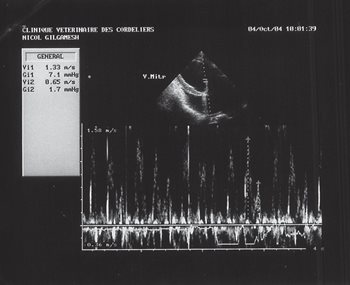 Figure 8: echocardiography (pulsed Doppler mode), left parasternal long axis image, four-chamber view: restrictive transmitral flow.
Figure 8: echocardiography (pulsed Doppler mode), left parasternal long axis image, four-chamber view: restrictive transmitral flow.
Echocardiography confirmed severe, mostly left-sided, chamber dilatation. The LA/Ao ratio was increased (figure 4) (LA/Ao = 2.7; normal < 1.6 [6]), as well as the LVEDD/Ao ratio (figure 5) (LVEDD/Ao = 3.1; normal < 1.8 [7]). Ventricular dilatation was also observed in M-mode during systole and diastole (figure 5) (LVEDD = 7.04 cm; normal < 4.4 cm [8]; LVESD = 4.04 cm;
normal < 2.9 cm [8]). The free side of the mitral valve leaflet was mildly thickened during diastole (figure 6) and systole (figure 7), and a small prolapse was seen (figure 7). Chordae tendinae were normal.
Transmitral flow was recorded in pulsed-wave Doppler echocardiography (figure 8) and showed a restrictive type (Appleton type 2, Em/Am= 2.04). A high velocity mitral regurgitation flow was recorded (Vmax=4.16m/s). All other flows (aortic, pulmonary and tricuspid) were within normal limits.
A haemotology and chemistry panel (BUN, creatinine, ALT, ALKP, glucose) were within normal limits.
The definitive diagnosis was mitral insufficiency responsible for grade 3a heart failure (ISACHC classification [9]), with alveolar pulmonary oedema and intermittent ventricular tachycardia.
Enalapril was maintained at the same dosage. Since the owners were not willing to leave the dog in the hospital, frusemide 4mg/kg divided BID [10] was prescribed for the pulmonary oedema, mexiletine 5mg/kg divided BID was prescribed for the arrhythmia [11], and pimobendan 0.5mg/kg divided BID was prescribed for its inotropic effect as recommended with at least grade 2 cardiac insufficiency [10,12].
The dog was presented for a recheck 10 days later. Clinical signs were markedly improved. Intolerance was observed only during moderate to marked effort. Heart rate was decreased and the rhythm was more regular. Respiratory signs were within normal limits.
An electrocardiogram (6 Leads, 25 mm/s, 10 mm/mV) (figure 10) showed marked improvement in the arrhythmia, with just a few isolated extrasystoles still being present. Chemistry panel (BUN, creatinine, ALT, ALKP, glucose, Na, K, Cl) was within normal limits. The treatment was maintained and the dose of frusemide was decreased from 4 mg/kg to 2 mg/kg.
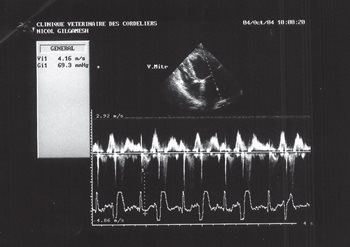 Figure 9: echocardiography (pulsed Doppler mode), left parasternal long axis image, four-chamber view: mitral regurgitation flow.
Figure 9: echocardiography (pulsed Doppler mode), left parasternal long axis image, four-chamber view: mitral regurgitation flow.
 Figure 10: electrocardiogram 6 Leads, 25 mm/s, 10 mm/mV: isolated left ventricular extrasystoles.
Figure 10: electrocardiogram 6 Leads, 25 mm/s, 10 mm/mV: isolated left ventricular extrasystoles.
A recheck was made over the phone 3 months later and no clinical signs were reported by the owners.
A recheck appointment to include radiographs, electrocardiogram and echocardiography was scheduled for 6 months later.